You waited… but now you’re wondering — is it too late to save my tooth?
That’s the exact moment people start searching. If you’re reading this, chances are you’re dealing with pain, swelling, or maybe your tooth just feels off. And you’re worried. We get it. Root canals can save teeth, but there’s a point where even that won’t help.
Let’s walk through how to tell when it’s too late for a root canal—and how to make sure you don’t get there.
When Is a Root Canal Needed? (And Why Timing Matters So Much)
Root canals treat infection and inflammation deep inside the tooth—what we call the pulp. This pulp can get damaged due to decay, trauma, or even repeated dental procedures. A successful root canal removes the damaged tissue, cleans the area, and seals the tooth.
✅ When done early, root canals have a success rate of 85–97%.
❌ But when done too late, you’re looking at extraction instead.
So, what’s “too late”? Let’s break it down clearly.
What Makes It Too Late for a Root Canal?
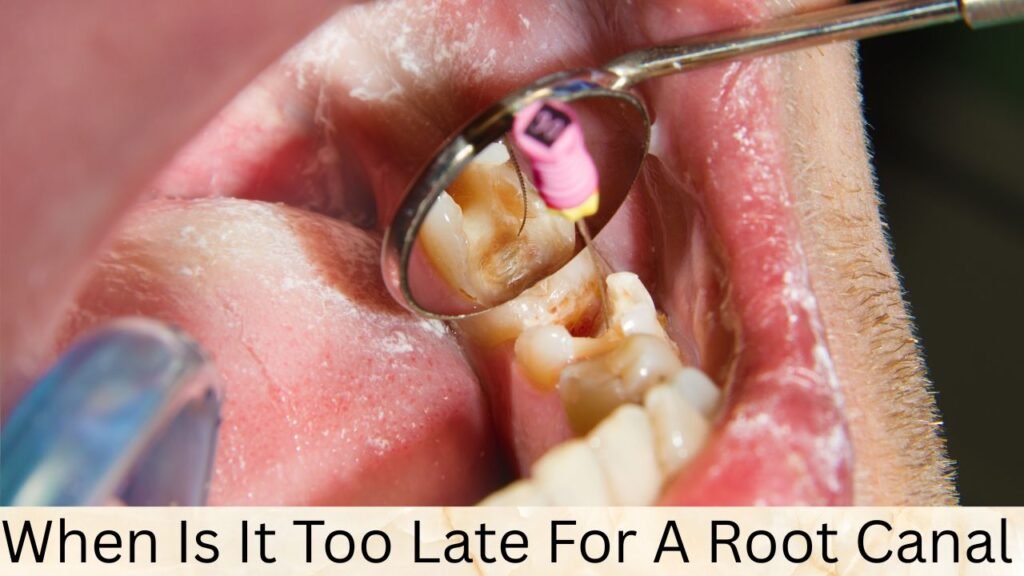
Dentists use both clinical exams and imaging—like CBCT scans or periapical X-rays—to evaluate a tooth. Here’s what they look for:
1. Advanced Pulpal Necrosis with Irreversible Inflammation
- When the pulp tissue inside the tooth has completely died, and bacteria has spread to the surrounding bone.
- You might feel pressure pain that doesn’t go away, even with meds.
Entities Involved: Pulp chamber, apical foramen, dentinal tubules.
2. Large Periapical Lesions
- These are infections that reach the tip of the root, causing abscesses or bone loss.
- Dentists see this on X-rays as dark, round areas.
- If left untreated too long, the surrounding bone can break down, making root canal therapy unreliable.
3. Tooth Root Resorption
- This happens when your body starts “eating away” the tooth structure—either from the inside (internal) or outside (external).
- Sometimes it’s painless until it’s too late.
- Once resorption is extensive, there’s no healthy structure left to save.
4. Tooth Mobility You Can Feel
- If the tooth is loose or shifting, that’s a red flag.
- Mobility means the bone around it may be severely compromised.
- In these cases, even if a root canal is technically possible, the prognosis is poor.
5. Persistent Swelling or a Gum Boil
- Recurring swelling, especially if it doesn’t go away with antibiotics, often means the infection is deep and chronic.
- These fistulas or “gum pimples” are signs the body is draining infection—and that it’s been doing so for a while.
🟨 Quick Table: Is a Root Canal Still Possible?
| Symptom or Sign | Root Canal Possible? | Prognosis |
|---|---|---|
| Mild to moderate pain, early decay | ✅ Yes | Excellent |
| Deep decay, no bone loss | ✅ Yes | Good |
| Periapical lesion <5mm | ✅ Possible | Fair to Good |
| Severe bone loss, visible resorption | ❌ Unlikely | Poor |
| Tooth mobility + chronic infection | ❌ Contraindicated | Poor |
The “Window of Opportunity” – What You Don’t Want to Miss
Early-stage pulpitis (inflammation of the pulp) is your best shot. If you catch it when you’re just dealing with cold sensitivity or occasional pain, the outcome is excellent. Here’s what ideal timing looks like:
- No visible bone loss yet
- Pain is intermittent, not constant
- No swelling or pus
- Tooth feels stable
- X-rays don’t show periapical pathology
💡 Moral of the story? If something feels off—don’t wait. The longer the infection sits, the lower the chance of saving the tooth.
But What If It Is Too Late? (Let’s Talk Options)
If your dentist determines that a root canal won’t work, here’s what they’ll usually recommend:
1. Tooth Extraction
- Pros: Stops the infection fast; simple procedure
- Cons: You’ll have a gap, jawbone loss can occur without a replacement
2. Dental Implant
- Pros: Long-lasting, preserves jawbone, looks natural
- Cons: Costly, requires healing time (3–6 months), surgery involved
3. Dental Bridge
- Pros: Faster than implants, good esthetics
- Cons: Involves shaping adjacent healthy teeth, may not last as long
4. Partial Denture
- Pros: Affordable, non-surgical
- Cons: Removable, less stable, not ideal for long-term use
Systemic Risks of Ignoring Advanced Dental Infections
Letting a deep infection go untreated can be dangerous. We’re not just talking about losing a tooth—bacteria can enter your bloodstream and contribute to:
- Endocarditis (heart inflammation)
- Respiratory infections
- Diabetes complications
- Brain abscesses (rare, but real)
So no, that “bad tooth” won’t just deal with itself.
Myth: “If It Doesn’t Hurt Anymore, It Must Be Fine”
Actually, this is one of the worst assumptions people make.
When the nerve dies, the pain might fade—but the infection keeps spreading silently. That’s why regular dental exams and diagnostic tools like CBCT scans are so important. Dentists can spot what you can’t feel.
Can Patients Tell It’s Too Late? (Some Clues You Can Spot)
While the final decision is up to your dentist, you might notice:
- Gum boils that come and go
- A bad taste in your mouth
- Looseness in the tooth
- Pain that spreads to the jaw or ear
- Swelling that never really resolves
If you’re experiencing more than one of these—call your dentist now, not later.
Prevention: How to Stay Ahead of the Curve
Want to avoid ever having to ask “Is it too late?” Here’s what helps:
- Annual digital X-rays
- CBCT scans when pain is vague or symptoms are inconsistent
- Cleanings every 6 months
- Early fillings before cavities go deep
- Don’t ignore temperature sensitivity
And when in doubt? Always ask.
Conclusion:
Here’s the truth: Only a dentist can tell you for sure if it’s too late for a root canal. But you don’t have to wait until it’s obvious. Every day matters. Even a tooth that seems hopeless might still be saved with the right timing and care.
So if you’re asking the question, that’s already your sign. Get checked. Don’t guess.
Find Your Perfect Dentist
Easily book appointments with top-rated dentists in your area
Need Emergency Dental Care?
Get immediate help from verified dental professionals