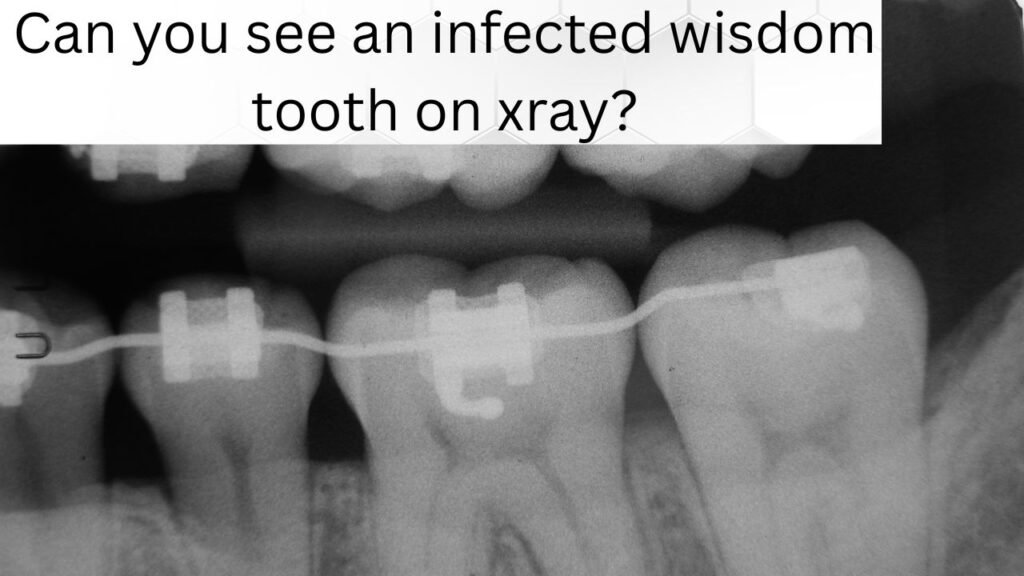
Can an X-ray show infected wisdom tooth problems? Many patients ask this when pain starts at the back of the mouth. Dental X-rays help dentists detect infection, bone loss, and impaction. Understanding what X-rays reveal helps you know when treatment or removal may be needed.
What an X-Ray Reveals About an Infected Wisdom Tooth
Dental X-rays are one of the best tools for diagnosing dental infections, especially for wisdom teeth that are hard to access. But not all infections show up the same way. Let’s explore the specific radiographic signs that dentists look for when they suspect an infected wisdom tooth.
Radiographic Signs of Infection: What to Look For
When it comes to wisdom teeth infection, there are several tell-tale signs on an X-ray that suggest something isn’t right. While periapical lucency and widening of the periodontal ligament space are well-known indicators, there are other specific patterns that might point to infection.
Periapical Lucency: A Key Indicator of Infection
Periapical lucency appears as a dark spot near the root tip on an X-ray. This is often the first sign of infection, where bacteria have caused bone loss around the root. However, not all dark areas mean infection. The size, shape, and location of the lucency are key factors in distinguishing infection from other lesions.
- Size and Shape: A larger, irregular-shaped lucency typically points to an infection, especially if it’s asymmetrical. Cysts and tumors might also show as radiolucent areas, but their shape and border characteristics are different.
- Location: If the lucency is located near the tooth apex (tip of the root), it’s more likely to be infection. A cyst or benign growth would typically appear in different locations.
Widening of the Periodontal Ligament Space: Inflammation at the Root
The periodontal ligament (PDL) space is a thin line seen between the tooth and surrounding bone. When infection occurs, this space can widen due to inflammation and the presence of inflammatory exudate (fluid released by the body during inflammation). This widening is caused by edema (swelling) around the root and is often one of the first visible signs of infection.
Bone Loss: Acute vs. Chronic Infections
This YouTube video below from 5MinuteSchool explains acute and chronic osteomyelitis in a clear, simple way. It covers causes, symptoms, and treatment differences. The overview helps readers understand this serious bone infection and its care.
Bone loss is another key indicator of infection, but its pattern can tell dentists whether the infection is acute or chronic.
- Acute Infections: In the early stages, bone loss is more localized and might appear as a sharp, focused area around the tooth. This can also lead to sudden pain and swelling.
- Chronic Infections: Over time, if the infection persists, the bone loss tends to be more diffuse and irregular. Chronic infections can cause severe bone destruction, which might even affect nearby teeth.
Sinus Tract: An Indirect Sign of Infection
In more severe cases, the infection might create a sinus tract, a small tunnel formed by the infection as it drains pus. Though X-rays can’t directly show pus or fluid, the sinus tract can sometimes appear as a faint radiolucent line extending from the infected tooth to the surface of the gums. This can be an indirect sign that the infection has become more severe.
Proximity to Vital Structures: What X-Rays Reveal About Nearby Nerves and Sinuses
Another important consideration when evaluating wisdom tooth infections is their proximity to vital structures, like the inferior alveolar nerve (in the lower jaw) or the maxillary sinus (in the upper jaw). Infected wisdom teeth can affect these structures, causing additional complications.
- Inferior Alveolar Nerve: On an X-ray, the nerve appears as a dark line running along the jaw. An infection near this nerve can cause numbness or tingling in the lower lip and chin, and may show up on the X-ray as bone loss or changes in the nerve’s position.
- Maxillary Sinus: For upper wisdom teeth, infection can spread to the sinus. This may be visible as changes in the sinus lining or bone around the tooth root, which could indicate sinus involvement.
Soft Tissue Involvement: Can You See It on an X-Ray?
While soft tissues like gums and internal swelling aren’t visible on traditional X-rays, sometimes dentists can spot calcifications in soft tissues near an infected wisdom tooth. These calcifications are small, hardened deposits that may form in response to long-standing inflammation. They can appear as tiny white spots in the soft tissue area surrounding the tooth.
In more severe cases, contrast-enhanced radiography (which uses a special dye) can help highlight soft tissue inflammation and areas where the infection may have spread into the surrounding tissues. However, this is not commonly used for routine wisdom tooth infections.
Stage of Wisdom Tooth Development: How It Affects the X-Ray Appearance
The stage of development of your wisdom tooth can also influence how an infection shows up on an X-ray. Here’s how:
- Impacted Wisdom Teeth: If the tooth is still embedded within the bone (impacted), the infection may not show up as clearly until the bone starts to break down. The X-ray will focus on the bone surrounding the tooth, showing changes in the bone structure.
- Partially Erupted Wisdom Teeth: For partially erupted wisdom teeth, infection is often more visible. You may notice signs of pericoronitis (gum infection), and the X-ray will show the surrounding bone, potentially revealing localized infection.
X-Rays vs. Clinical Signs: Why Both Matter
It’s important to understand that X-rays can’t always detect every stage of an infection. Early signs, such as mild gum irritation or small amounts of bone loss, may not be visible immediately. That’s why a clinical examination (your dentist’s assessment of your symptoms and physical exam) is just as important as the X-ray itself.
Additionally, X-rays are limited by their inability to show soft tissue details or subtle inflammation. False negatives are possible, where an infection isn’t visible on the X-ray despite clear clinical symptoms. That’s why it’s essential for the dentist to correlate X-ray findings with your symptoms.
What Should You Look for in Your X-Ray Report?
When reviewing your X-ray report, there are a few key things to focus on, especially if you’re concerned about infection:
- Radiolucent Areas: Check for any dark spots around the tooth roots that may suggest infection.
- Bone Loss: Look for any changes in the bone structure around the tooth. Significant loss is a clear sign of an ongoing infection.
- Periodontal Ligament Space: A widened PDL space is an early indicator of infection.
- Proximity to Nerves or Sinus: This will help determine if the infection could spread and affect vital structures.
Follow-Up X-Rays: Tracking Healing or Progression
After treatment for an infected wisdom tooth, follow-up X-rays are often necessary to monitor healing. These X-rays help the dentist ensure that the infection is resolving and that there are no lingering issues, such as bone loss or abscess formation.
Conclusion:
So, can an X-ray see an infected wisdom tooth? Yes, it can—but it’s not always the whole story. X-rays are a powerful tool in detecting signs of infection, such as periapical lucency, widened periodontal ligament space, and bone loss, but they don’t show everything. Early infections or soft tissue inflammation might not be visible. That’s why it’s crucial for your dentist to consider both your X-ray results and clinical symptoms when making a diagnosis.
If you’re concerned about a possible infected wisdom tooth, don’t hesitate to visit your dentist. With the right combination of X-rays and clinical expertise, they can pinpoint the issue and recommend the best course of action to relieve your pain and prevent further complications.
Find Your Perfect Dentist
Easily book appointments with top-rated dentists in your area
Need Emergency Dental Care?
Get immediate help from verified dental professionals